
Contentnesthub
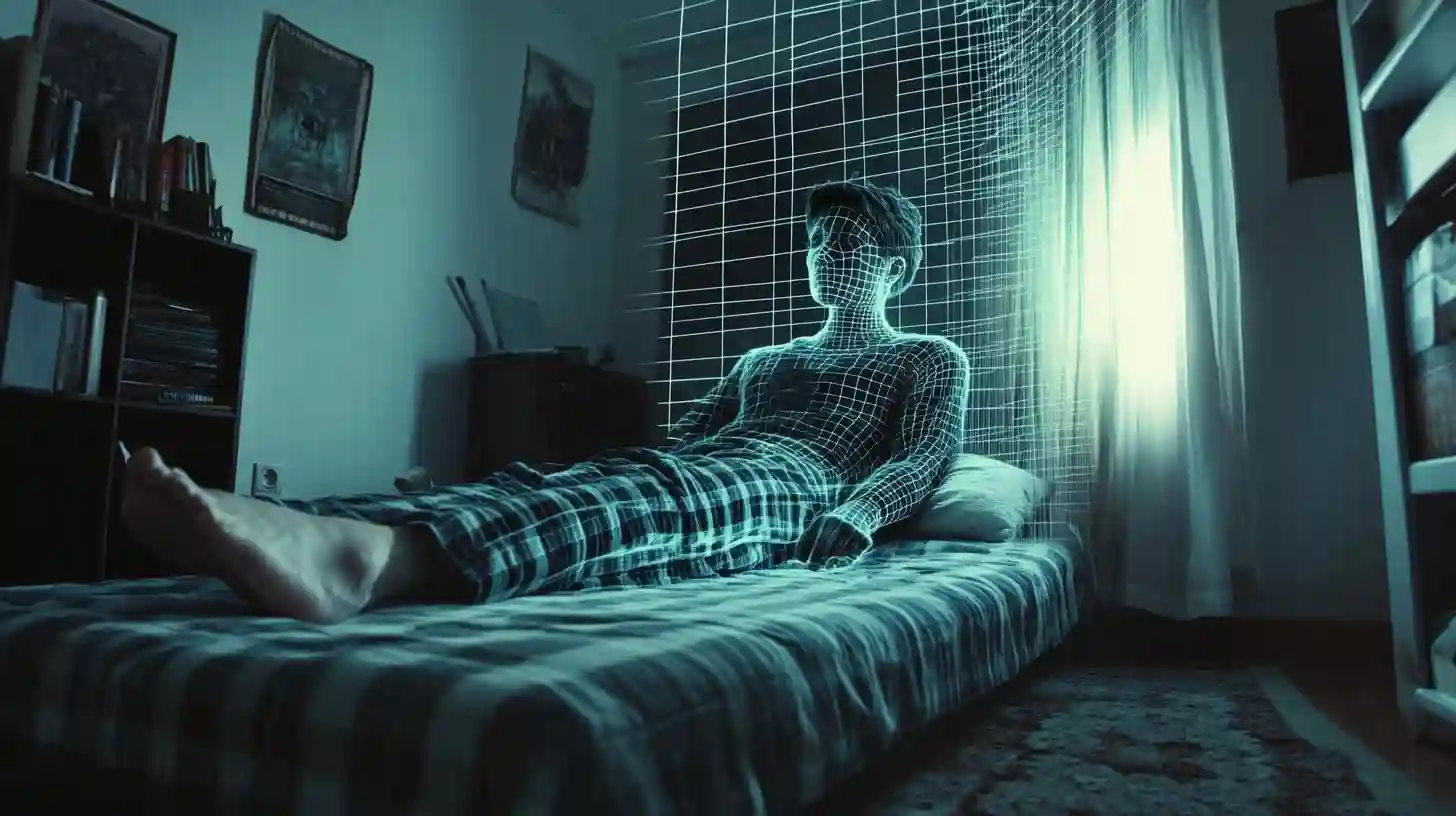
Sleepwalking, a phenomenon characterized by walking or performing other complex behaviors while still in a state of sleep, has long intrigued researchers, medical professionals, and the general public alike. This episode of parasomnia occurs predominantly in children but can also be experienced by adults. To grasp the underlying factors contributing to this unusual sleep behavior, it is essential to delve into the complexities of sleepwalking, including its causes, potential risk factors, and the implications it holds for those who experience it.
The sleep cycle is composed of various stages, primarily divided into non-rapid eye movement (NREM) and rapid eye movement (REM) sleep. Sleepwalking typically arises during the deep stages of NREM sleep, specifically in the transition from deep sleep to lighter sleep phases. At this point, the brain remains partially active while the individual remains largely unaware of their surroundings. This disconnection can result in actions such as walking, opening doors, or even attempting to engage in routine activities, all while remaining in a somnolent state.
A significant factor contributing to sleepwalking behavior is genetics. Studies have indicated that sleepwalking can run in families, with a higher incidence of the disorder observed among those who have family histories of sleepwalking or other parasomnias. Research has suggested that certain genetic factors may predispose individuals to sleep disturbances, including inconsistent sleep patterns and other sleep disorders. Identifying a hereditary aspect to the condition provides valuable insight, indicating the potential for biological predispositions to influence sleep behavior.
Moreover, environmental factors can exacerbate or trigger sleepwalking episodes. Conditions such as sleep deprivation, fatigue, or irregular sleep schedules can contribute to disturbances in sleep patterns, increasing the likelihood of sleepwalking. Stress and anxiety are also concurrent triggers; emotional stressors can disrupt normal sleep, leading to episodes of sleepwalking. Changes in a routine, significant life events, or even daily pressures can affect sleep quality, heightening the risks of experiencing an episode.
In addition to external and environmental factors, certain health conditions have been linked to sleepwalking behavior. For instance, individuals suffering from obstructive sleep apnea—a condition that results in repeated interruptions in breathing during sleep—may display increased occurrences of sleepwalking. Other medical conditions such as seizures, restless leg syndrome, and even insomnia can contribute to heightened vulnerability to parasomnias. Moreover, medications affecting the central nervous system can also provoke sleepwalking as a side effect, illustrating the intricate relationship between various health factors and sleep behavior.
Sleepwalking can manifest in different forms, leading to varying degrees of severity and potential implications. While some individuals may experience benign episodes that pose little risk, others may engage in more dangerous behaviors, leading to injuries to themselves or others. Importantly, sleepwalkers are often unable to recall their actions upon waking, which can further complicate matters if they find themselves in precarious situations. Fortunately, most individuals who experience sleepwalking eventually outgrow it, particularly if it begins in childhood. However, for those who continue to experience episodes into adulthood, the implications can extend beyond physical safety.
The risks associated with sleepwalking behaviors cannot be overstated. Individuals may inadvertently place themselves in dangerous situations, such as leaving their homes or operating vehicles while asleep. Cases have been documented of individuals getting into accidents or engaging in aggressive or harmful behaviors during episodes, leading to legal ramifications in some cases. The unpredictability of sleepwalking has led to concerns regarding personal safety, necessitating proactive measures and strategies to mitigate risks.
Beyond the physical implications, sleepwalking can significantly impact the quality of life for both the individuals who experience it and their families. Families of sleepwalkers often endure heightened anxiety regarding their loved ones’ safety during sleep. The fear of finding a family member engaging in potentially harmful behaviors can disrupt the tranquility of the household. Additionally, social implications arise as individuals may experience embarrassment or shame surrounding their condition. This can lead to social withdrawal or avoidance of situations where sleepwalking may occur, such as sleepovers or communal living environments.
Mental health considerations are also an essential aspect to address in discussions concerning sleepwalking. Research has shown that sleepwalking episodes may correlate with underlying psychological issues such as anxiety, depression, or post-traumatic stress disorder. The nuances of this relationship indicate a complex interplay between mental health and sleep behavior, where psychological factors may either influence sleepwalking or arise as a consequence of the condition itself. Addressing mental health is vital in both the prevention and management of sleepwalking episodes, emphasizing the need for a holistic approach to treatment.
The diagnosing and treatment of sleepwalking can take several avenues. First, healthcare professionals typically gather comprehensive sleep histories, assessing patterns and potential triggers associated with episodes. Polysomnography, a study conducted during sleep, can also assist in diagnosing sleep disorders, providing valuable insights into the sleep stages and disturbances that may be occurring. Treatments may include lifestyle changes such as establishing consistent sleep routines, ensuring adequate sleep hygiene, and addressing environmental stressors that may exacerbate the condition.
In certain cases, cognitive-behavioral therapy might be recommended to address underlying psychological factors contributing to sleepwalking episodes. In instances where medication is necessary, physicians may employ medications that promote stable sleep patterns and reduce the likelihood of parasomnias. Equally important is the crafting of a safe sleep environment. This can involve restricting access to potentially hazardous areas of the home and ensuring that sleepwalkers are not left unattended during the night.
Educational efforts should also focus on raising awareness about sleepwalking and its implications. Misinformation and stigma can exacerbate the challenges individuals face when dealing with sleepwalking. Cultivating understanding among peers, family members, and the community can foster supportive environments where individuals feel empowered to seek help and discuss their experience without fear of judgment.
As ongoing research continues to explore the dimensions of sleepwalking and its causes, the field gains deeper insights into this complex behavior. Understanding the relationship between genetics, environmental triggers, and health conditions will be crucial as society seeks to address the needs of those who experience sleepwalking. With collaborative efforts from healthcare professionals, researchers, and advocates, individuals who walk in their sleep can find pathways to safer, more restful experiences. The key lies not only in managing episodes but also in fostering a deeper understanding of sleep as a fundamental component of health and well-being.